Why Conflict Doesn’t Need to Mean Cut-Off
In the northeastern corner of Nigeria, bordering Cameroon to the east and Niger to the north lies Borno state. Home to over 4 million people, the area is infamous for the war that has been raging for over a decade. Since 2009, Borno state has been the epicenter of the Boko Haram insurgency. Since the rise of the conflict, Borno’s inhabitants have lived with the ever-present danger of violence, kidnapping and loss of life, as witnessed globally by the kidnapping of 276 Chibok schoolgirls in 2014. Over half of the state’s inhabitants have lost their homes and primary livelihoods and remain displaced people in a land that once offered stability and opportunity. Yet despite the difficulty of existence in a conflict zone, life with all its attendant expectations must somehow carry on. Food must be planted and harvested, livelihoods must be managed, people must marry and as children are born, they must still be vaccinated.
Within Borno, the State Primary Health Care Development Agency (Borno SPHCDA) remains responsible for delivering health services to its population.
Key Facts
Over 50% of children in Borno state are in conflict zones
Large pockets of people live in insurgent-held territories
Access to health care and immunization services in many communities has been cut off since 2013
However, large pockets of people live beyond the government safe zones in insurgent-held territories rendering them extremely vulnerable. Dishearteningly, the states’ health center infrastructure had been decimated over the years, making service delivery in some areas difficult and almost impossible in other areas. With the escalation of conflict, immunization coverage had fallen sharply to 12% by 2013, compelling the Borno SPHCDA to creatively address the question of how to reach vulnerable children, cognizant of the continued insecurity wrought by the conflict. Lessons from an ongoing strategy to expand access to polio vaccines known as Reaching Inaccesible Children (RIC) offered a valuable starting point.
Main Challenges
Access to care in a conflict zone
Conflict zones have low immunization rates
SPHCDA was clear that while provision of health services was its mandate, delivery in a situation defined by constantly changing variables posed a conundrum that was beyond its scope. Incorporating new allies in the quest to achieve routine immunization goals was necessary if they were to turn around the fast-declining vaccination coverage. As a result, SPHCDA worked with three core implementation initiatives that each brought in specific expertise to tackle low vaccination coverage. In addition, SPHCDA received vaccine and related supplies from National Primary Health Care Development Agency (NPHCDA), commodities from UNICEF while WHO provided supervisory support.
Insights
Purpose in Planning: One of the early core implementation groups SPHCDA worked with was the Solina Center for International Development and Research (SCIDaR), a Nigerian non-profit institution focused on promoting positive health and social well-being across the country. With a bias towards impact and focus on crafting homegrown solutions, the institution has been at the forefront of seeding change in unlikely places – such as Borno.
Technology: The second group was eHealth Africa, a global technology firm that could provide real time information on where to find mobile populations based on GIS coordinates and migration mapping within the conflict hot zones.
Security: The final critical task was to identify personnel to provide security for the health worker teams and patients. Building off learnings from polio eradication, SPHCDA knew that the required security was two-fold: it involved both protection and intelligence gathering. Communities had developed a Civilian Joint Task Force (cJTF) that worked with the military, community vigilante groups and religious and local leaders to provide cover and insights on safety measures and community movements.
Together, this unusual collective proceeded to break down the challenges facing vaccination delivery, the most critical being the lack of physical structure through which they could deliver their work. Many health facilities were bullet ridden shells, offering no protection for service delivery.
Security Analysis
Analyze levels of insecurity to understand go-zones vs. no-go zones.
Develop two-fold approach of protection and information gathering.
The teams strategized and developed two options for service – the first was a strategy for delivery in insurgent held areas. Known as the “hit and run” approach, the teams would venture into a community in rebel-held areas, assemble all children under five, quickly identify their immunization needs and provide the requisite vaccinations within the shortest time possible. The deftly executed services would be complete within a few hours. A second option was designed for more stable areas where a security detail from the cJTF would provide key information for safe zones for the health team to set up a temporary health post known as a “fixed post” within a two-kilometer radius from several villages or settlements. At these fixed posts, basic health services including immunization would be provided over a 4-6 hour period before the post was disassembled and the team deployed back to a safe zone. The GIS team’s information would be critical for this effort, ensuring that communal sites could serve as many people as possible. This two-pronged approach enabled the team to turn around the dwindling coverage numbers in several settlements from 2017.
| Number of Unimmunized Children in Select Settlements in Borno | ||
|---|---|---|
| Q4 2017 | Q3 2019 | |
| Damboa | 57 | 15 |
| Dikwa | 60 | 12 |
| Kaga | 57 | 49 |
| Magumeri | 59 | 13 |
| Nganzai | 60 | 15 |
Despite these supply solutions, the team still faced serious challenges including: fear amongst health workers to deploy into rebel-held territory; a compromised immunization information chain resulting from the reluctance of mothers to hold onto immunization cards for fear of them being found by Boko Haram; difficulty in maintaining the vaccination schedule due to timings on account of shifting concerns; and rumors and myths about vaccination cropping up in selected areas that dampened demand.
Yet, since the development of this approach, marked improvements have been seen in the locations. Since 2018, a continued rise in the number of children that have received the complete immunization regimen has been recorded. Meanwhile despite the potential risk of being seen as a government supporter by insurgents, more and more community members have taken up the government- provided health services that ride on the fixed post strategy.
Immunization Options
“Hit and Run”
Minimal time spent in communities to reduce vulnerability of attack. Only vaccination was offered.
“Safe fixed post”
Require cJTF to put in place a security perimeter located on a 2km radius from the majority of homes in the area. All primary health care (PHC) was offered including vaccination.
Results
The percentage of settlements having been served more than once
The percentage of children vaccinated in the March 2020 routine immunization expansion round
The average percentage of children reached by routine immunization expansion teams per round between April and December 2019
1831 out of 1989 settlements have been served.
Like many hotspots across the globe, Borno state has been in the unenviable position of having to craft solutions for increasing access to and use of care under the most difficult of circumstances. Yet the team at SPHCDA and their partners are bringing hope to those who need it most, through a partnership that leverages new technology and age-old systems of community resilience. Approaches like theirs remind us that there is still hope for the vulnerable when health becomes the responsibility of a wider community.
Immunization Insights
Beyond Vaccines: In conflict zones, immunization services should be offered within the context of primary health services. Communities are likely to place greater value on receiving healthcare services and providing immunization services from the same health workers building valuable connections between communities and providers. The outcome? More households bringing their children in for vaccination while seeking basic medical consultations.
Recognizing Expertise: Given the fluidity of the security situation, the SPHCDA leaned into the advice and experience of non-health actors including security agents. The value of partnerships that bring in varied expertise that enabled or helped accelerate delivery was critical in the achievement of SPHCDA’s mandate
Healthworkers First: Working in a conflict zone requires a heightened level of commitment from health workers. The collaborative led by SPHCDA took time to engage with the on-the-ground teams and develop interventions that allay health workers’ concerns. This gave healthworkers the peace of mind to put in their best efforts in the two delivery scenarios.
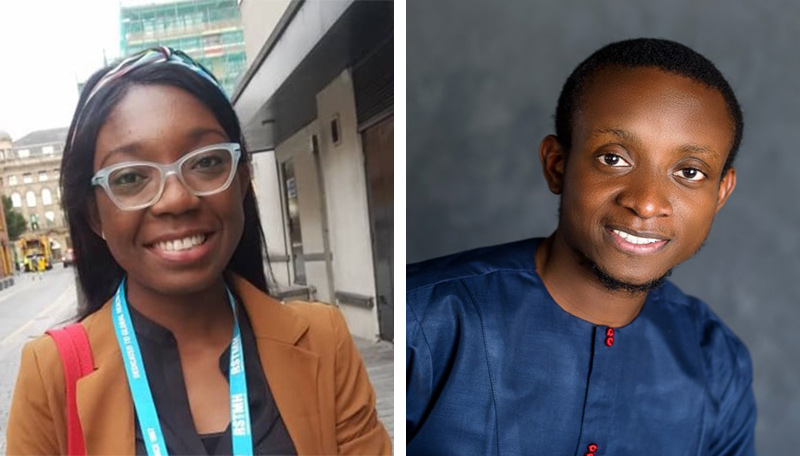
Teslim Aminu and Adetola Oladimeji
This Bright Spot story was nominated by Teslim Aminu and Adetola Oladimeji, Managers with Solina Center for International Development and Research (SCIDaR) in Nigeria. They hope that this story will be helpful to others working to expand routine immunization coverage in conflict areas


